Deliver Better Care with Accurate Quality Reporting
Streamline your reporting process, meet compliance standards, and improve patient outcomes with our comprehensive quality reporting solution
Ensuring Excellence Through Data-Driven Reporting
Quality reporting in healthcare can be the foundation of a solid business plan and a commitment to better patient care. By identifying and tracking clinical quality measures, your healthcare organization can deliver better value-based care, meet reporting requirements, benefit from incentives designed to reward improved healthcare quality and reduce the overall cost of care.
Quality reporting is a critical aspect of modern healthcare, enabling you to track, evaluate, and report on care quality metrics. Our solution simplifies this process by consolidating data from multiple sources, automating calculations, and ensuring compliance with industry standards like MIPS, MACRA, and HEDIS.
How Quality Reporting Impacts Healthcare Workflows
When adopting quality reporting into your daily operations, you may face various drawbacks, such as spending extra time entering data and consistently ensuring the accuracy of the information. At Graphite, we offer Analytics tools for accurate and efficient quality reporting.
Our analytic tools enable you to identify patterns and areas for improvement. It saves time and facilitates better workflows.
This quality reporting tool integrates with almost any electronic health record (EHR) system for gaining valuable insights into your processes and accurate reporting. In addition to monitoring quality measures, you can quickly respond to gaps and issues in your workflow to ensure your organization continues to deliver high-quality value-based care.
By integrating with an EHR system, you can automate much of the clinical quality reporting process. Strictly observing data quality control and monitoring regularly should ensure you pull the appropriate data from your records.
The Role of MIPS in Healthcare Quality Reporting
Merit-based Incentive Payment System (MIPS) oversees a quality payment system that uses value-based care metrics to reward healthcare providers and organizations that provide Medicare Part B services. Requirements include a mandate to take part in quality reporting and show year-over-year quality improvement.
Quality measurement reporting requirements can vary from organization to organization. Most organizations can select specific areas to focus on, targeting the outcome measure for each area to show improvement and raise their quality score.
Individual care providers and group practices, clinics, or other healthcare facilities can benefit from submitting an annual quality report. Besides incentives offered through MIPS, this quality data can help leverage better reimbursement rates from independent insurers while improving efficiency and the overall quality of care.
Quality Reporting Benefits
Better Healthcare Quality
When you engage in quality reporting, any issues with patient care and outcomes will come instantly to the surface, where you can deal with them. You can also measure the effectiveness of your efforts and take steps to address any areas that require improvement. The result is better quality care and more positive outcomes for the patients you serve
Improved Coordination
Quality reporting systems enable clinically integrated networks (CINs) and accountable care organizations (ACOs) to gather data across various organizations and simplify collective reporting and analysis. These organizations are only as strong as their members. Happe-Analytics connects with virtually any EHR system, making it easy to measure performance and work toward upgrading care outcomes while reducing costs.
Reduced Cost of Care
Value-based care does not mean cutting corners; rather, it is a commitment to providing higher value to patients at a lower cost by being proactive about patient care. Diagnosing and treating potential or emergent issues early on can improve the overall well-being of a patient. This can also delay or stop additional or related problems before they cause a deterioration in patient health, resulting in cost savings down the line.
Increased Revenues
Quality reporting is a relatively easy and foolproof way to improve MIPS scoring for top-tier incentives and maximize your reimbursements from other value-based programs. The result is a better bottom line for your organization.
The Future of Quality Reporting
Modern quality reporting involves leveraging the wealth of patient data at your organization. A good place to start is to implement a physician quality reporting system. The next step is to identify and record relevant healthcare quality measures so you can track improvements.
As the parameters for value-based care reporting continue to change annually, being able to use a 360-degree view of your organization’s data, from patient populations to outcomes to financials, is key to success. Aside from receiving reimbursements and financial incentives, quality reporting helps your organization uphold clinical guidelines and standards and implement the best practices for your healthcare specialization.
The goal is to provide proactive and value-based healthcare, maximizing patient outcomes and minimizing costs. You need to be more than just a healthcare organization, but a quality improvement organization focused on continually raising the bar for both your patients and your bottom line.
A quality reporting system designed for meaningful use under MIPS guidelines will deliver reports that keep you in compliance and earn top scores year after year.
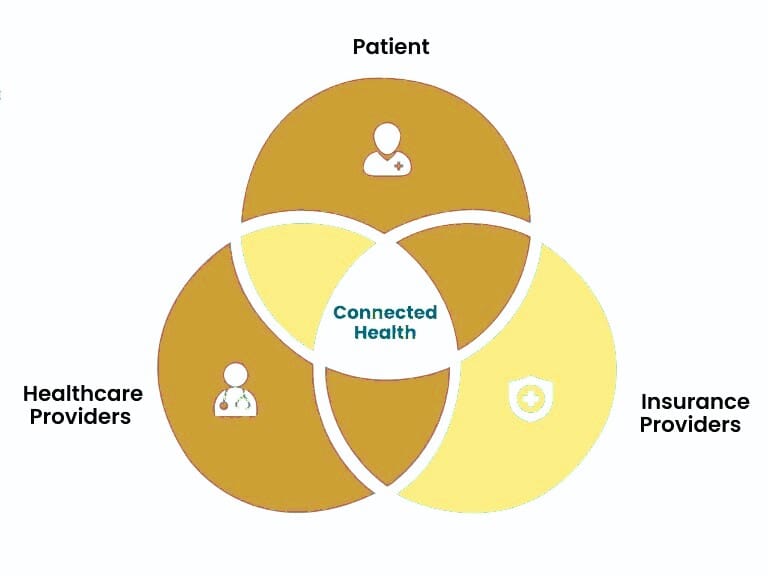
Achieving top scores goes beyond the number of services you provide — you must take a value-based approach to reach those quality measures. Value-based care helps reduce healthcare costs, improve patient satisfaction and engagement, and facilitate seamless coordination among healthcare providers, specialists and stakeholders.
Whether you are a singular healthcare provider, managing a home health organization, or running a major hospital, quality reporting is the path to meeting healthcare quality goals and maximizing revenues.